Your Cart is Empty

ইরিটেবল বাওয়েল সিনড্রোম (আইবিএস) কি আপনাকে ব্যথা, ফোলাভাব এবং বিব্রতকর হজমের লক্ষণগুলির সাথে লড়াই করতে দেয়? কৌশলগত খাদ্য পরিবর্তনের মাধ্যমে মুক্ত হতে চান? একটি IBS চিকিত্সা খাদ্য পরিকল্পনা ট্রিগার সনাক্ত করতে এবং ত্রাণ খুঁজে পেতে সাহায্য করতে পারে।
গবেষণা দেখায় যে আপনি যা খান তা পরিবর্তন করা ইরিটেবল বাওয়েল সিন্ড্রোমকে উল্লেখযোগ্যভাবে প্রভাবিত করে। যাইহোক, সর্বোত্তম পন্থাগুলির বিরোধপূর্ণ তত্ত্বগুলির সাথে, আইবিএস চিকিত্সার জন্য আপনার সর্বোত্তম খাদ্য পরিকল্পনা আবিষ্কার করতে পরীক্ষা এবং ত্রুটির প্রয়োজন হতে পারে।
যাইহোক, চিন্তা করবেন না! কম FODMAP থেকে কম চর্বি পর্যন্ত এই ব্লগটি আপনাকে কার্যকরী, প্রমাণ-ভিত্তিক IBS ডায়েটের মাধ্যমে পরীক্ষা করবে। এটি আপনাকে একটি IBS চিকিত্সা খাদ্য পরিকল্পনা তৈরি করতে সাহায্য করবে যা আপনার জন্য অনন্যভাবে তৈরি করা হয়েছে।
কিছু প্রমাণ-ভিত্তিক খাদ্য পদ্ধতি রয়েছে যা নাটকীয়ভাবে আইবিএস লক্ষণগুলিকে উন্নত করতে পারে। আপনার নির্দিষ্ট ট্রিগার এবং উপসর্গের উপর নির্ভর করে, বিকল্পগুলি অন্তর্ভুক্ত করতে পারে:
কম FODMAP ডায়েটটি মূলত অস্ট্রেলিয়ার মেলবোর্নের মোনাশ বিশ্ববিদ্যালয়ের গবেষকরা তৈরি করেছিলেন। তারা দেখেছেন যে কম গাঁজনযোগ্য কার্বোহাইড্রেটযুক্ত খাবার আইবিএস রোগীদের পেটে ব্যথা, ফোলাভাব, কোষ্ঠকাঠিন্য এবং ডায়রিয়ার মতো লক্ষণগুলিকে উল্লেখযোগ্যভাবে উন্নত করে।
FODMAP শব্দটির অর্থ হল:
এফ - ফার্মেন্টেবল - যার অর্থ তারা জলকে আকর্ষণ করে এবং অন্ত্রের ব্যাকটেরিয়া দ্বারা দ্রুত গাঁজন হয়
O - Oligosaccharides - Oligosaccharides হল কার্বোহাইড্রেট চেইন যা তিন থেকে দশটি সরল শর্করা (monosaccharides নামেও পরিচিত) দিয়ে তৈরি।
ডি - ডিস্যাকারাইডস - ল্যাকটোজ সহ কার্বোহাইড্রেটের একটি গ্রুপ।
এম - মনোস্যাকারাইডস - অতিরিক্ত ফ্রুক্টোজ সহ কার্বোহাইড্রেটের একটি গ্রুপ।
ক - ও
P - পলিওল - শর্করার অ্যালকোহলের একটি গ্রুপ, যার মধ্যে রয়েছে সরবিটল, ম্যানিটল, জাইলিটল এবং ম্যাল্টিটল
এটি জটিল বলে মনে হতে পারে, তবে ধারণাটি সহজ - এই গ্রুপগুলিতে শর্ট-চেইন কার্বোহাইড্রেট রয়েছে যা ভেঙে ফেলা এবং হজম করা কঠিন হতে পারে। সঠিকভাবে শোষিত হওয়ার পরিবর্তে, তারা আপনার অন্ত্রে জল টেনে নেয়, ব্যাকটেরিয়া দ্বারা গাঁজন করে এবং অস্বস্তিকর উপসর্গ সৃষ্টি করে।
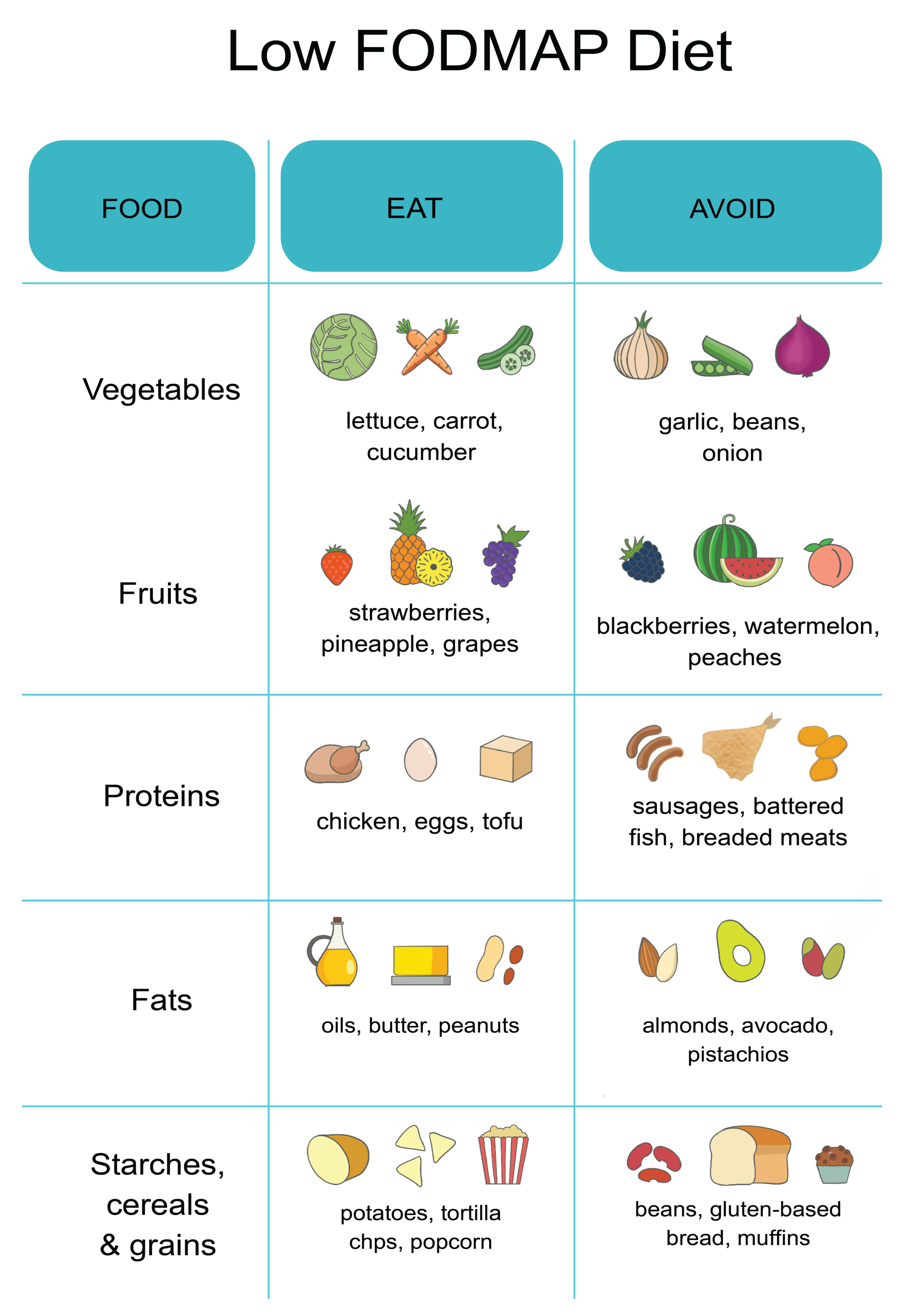
কম FODMAP ডায়েট 4-8 সপ্তাহের জন্য এই কার্বোহাইড্রেট সমৃদ্ধ খাবারগুলিকে বাদ দেয় । এটি অন্ত্রের প্রদাহ এবং ভারসাম্যহীনতা নিরাময় করতে দেয়। তারপরে নির্দিষ্ট খাবারগুলি প্রতি 3 দিনে পর্যায়ক্রমে সহনশীলতা পরীক্ষা করতে এবং আপনার ব্যক্তিগত ট্রিগারগুলি নির্ধারণ করতে পুনরায় চালু করা হয়। অনেকে দেখতে পান যে তারা ছোট পরিবেশনে কিছু উচ্চ-FODMAP খাবার উপভোগ করতে পারে।
যেহেতু শর্করা প্রধান ফোকাস, তাই শস্য, ফল, শাকসবজি, বাদাম, বীজ, লেগুম এবং দুগ্ধজাত খাবার যেখানে আপনি সবচেয়ে বেশি FODMAP খাবার পান। এখানে কিছু নির্দিষ্ট আছে:
যেকোনো সীমাবদ্ধ খাদ্যে ঝাঁপিয়ে পড়া চ্যালেঞ্জিং। পেশাদার নির্দেশিকা আপনাকে প্রক্রিয়াটিকে মসৃণ করতে সহায়তা করবে। এই টিপস এছাড়াও সাহায্য:
অধ্যয়নগুলি দেখায় যে একটি কম FODMAP ডায়েট আইবিএস চিকিত্সার জন্য খুব আশাব্যঞ্জক , 76% এরও বেশি ত্রাণ অনুভব করছে। তবে সীমাবদ্ধতার সাথে চ্যালেঞ্জও রয়েছে। এটি পুষ্টির দিক থেকে পর্যাপ্ত এবং টেকসই তা নিশ্চিত করতে একজন ডাক্তার এবং খাদ্য বিশেষজ্ঞের সাথে কাজ করুন। সবচেয়ে গুরুত্বপূর্ণ, ক্ষমতায়ন অনুভব করুন যে আপনি ডায়েটের মাধ্যমে লক্ষণগুলি পরিচালনা করতে পারেন।
নির্মূল খাদ্য একটি বর্ধিত সময়ের জন্য নির্দিষ্ট খাবার এড়িয়ে আইবিএস লক্ষণগুলি সনাক্ত করতে এবং সহজ করতে সহায়তা করে। এর অর্থ হতে পারে সম্পূর্ণ খাদ্যের বিভাগ কমানো, যেমন কম FODMAP ডায়েটে, অথবা পৃথক ট্রিগার খাবার এড়িয়ে যাওয়া।
এখানে কিছু সাধারণ আইবিএস ট্রিগার খাবারের একটি তালিকা রয়েছে:
দ্রষ্টব্য: আপনার উপসর্গগুলির জন্য একটি সম্ভাব্য ট্রিগার বলে মনে হয় এমন কোনও খাদ্য আইটেম বাদ দিয়ে পরীক্ষা করার পরামর্শ দেওয়া হয়।
বেশি ফাইবার গ্রহণ করা, বিশেষ করে দ্রবণীয় ফাইবার, যাদের আইবিএস-সম্পর্কিত কোষ্ঠকাঠিন্য রয়েছে তাদের উপকার করতে পারে। ফল, মটরশুটি, ওটস এবং কিছু শাকসবজি থেকে দ্রবণীয় ফাইবার মল তৈরি করতে সাহায্য করে এবং নিয়মিততা বাড়ায়।
চিকিত্সকরা প্রায়শই পরামর্শ দেন যে আইবিএস-এর রোগীরা মল নিয়ন্ত্রণ করতে এবং পেটে ব্যথা কমাতে তাদের দৈনিক খাদ্যতালিকাগত ফাইবার গ্রহণের পরিমাণ 20-35 গ্রাম বাড়ান । 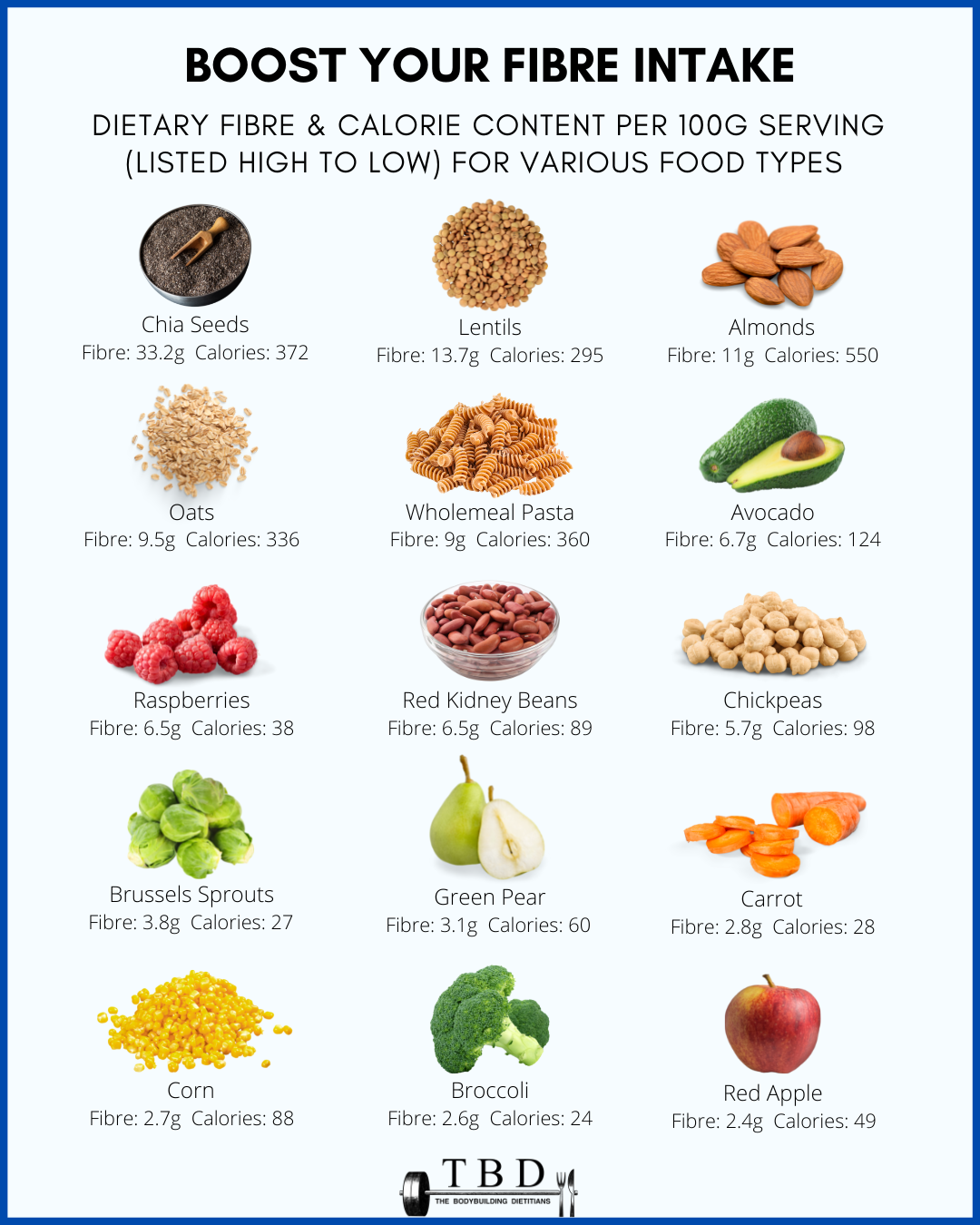
কোষ্ঠকাঠিন্যের সাথে মোকাবিলা করলে ধীরে ধীরে আপনার ফাইবার গ্রহণ বাড়ান। খুব দ্রুত বাড়লে অপ্রীতিকর গ্যাস এবং ফোলাভাব হতে পারে। প্রতিদিন 2-3 গ্রাম বেড়ে যান। ফাইবার সামগ্রিকভাবে স্বাস্থ্যকর হজমে সহায়তা করে, আপনার যদি আইবিএস থাকে তবে প্রথমে দ্রবণীয় উত্সগুলিতে ফোকাস করুন।
আপনি যদি এখনও ক্রমাগত গ্যাসের সম্মুখীন হন তবে সাইলিয়াম ভুসির মতো পরিপূরকগুলি অন্বেষণ করুন। যদিও আরও গবেষণার প্রয়োজন রয়েছে, কিছু গবেষণায় দেখা যায় যে পরিপূরক ফাইবারের প্রকারগুলি বিশেষভাবে আইবিএস কোষ্ঠকাঠিন্য থেকে মুক্তি দেয়।
আপনার যদি ডায়রিয়া-প্রধান আইবিএস থাকে, তবে উচ্চ ফাইবারযুক্ত খাবার সীমিত করা, বিশেষ করে অদ্রবণীয় ফাইবার সমৃদ্ধ, কখনও কখনও উপশম দিতে পারে। অদ্রবণীয় ফাইবারের উদাহরণগুলির মধ্যে রয়েছে জুচিনি, গোটা শস্য, টমেটো, বাদাম, ব্রোকলি এবং আরও অনেক কিছু। যাইহোক, ফাইবার এখনও প্রতিরক্ষামূলক হজম সুবিধা প্রদান করে।
এটি সম্পূর্ণরূপে নির্মূল করার পরিবর্তে, ওটস, গাজর, মটর এবং বেরিগুলির মতো দ্রবণীয় ফাইবারের উত্সগুলিতে মনোনিবেশ করুন। এই খাবারগুলি আরও সহজে দ্রবীভূত হয় এবং অদ্রবণীয় ফাইবারের সাথে আসা অতিরিক্ত বাল্ক যোগ করে না। সম্পূর্ণ শস্য, শাকসবজি এবং তুষের মতো অদ্রবণীয় ফাইবার সীমিত করুন, যা ডায়রিয়াকে আরও খারাপ করতে পারে।
এমনকি আপনার সিলিয়াক রোগ না থাকলেও, গ্লুটেন কেটে ফেলা এখনও আইবিএস লক্ষণগুলির সাথে সাহায্য করতে পারে। গম, বার্লি, রাই, ইত্যাদির মতো গ্লুটেন আছে এমন শস্যগুলি অপসারণ করার চেষ্টা করুন৷ এটি আপনাকে দেখতে সাহায্য করবে যে আপনার সংবেদনশীলতা আছে কিনা যা অন্ত্রের সমস্যা সৃষ্টি করতে পারে৷ 
একটি সমীক্ষায় দেখা গেছে যে 6-সপ্তাহের গ্লুটেন-মুক্ত ডায়েট 41 জন অংশগ্রহণকারীর আইবিএস সমস্যাগুলি উল্লেখযোগ্যভাবে হ্রাস করেছে। এবং 18 মাস পরে, যারা এখনও গ্লুটেন-মুক্ত তাদের জন্য লক্ষণগুলি উন্নত ছিল। এটি স্বল্প এবং দীর্ঘমেয়াদী উভয় সুবিধা নির্দেশ করে।
গ্লুটেন আপনার আইবিএসকে প্রভাবিত করে কিনা তা পরীক্ষা করার জন্য রুটি, সিরিয়াল, পাস্তা, ক্র্যাকার এবং বিয়ারের মতো আইটেমগুলি কেটে ফেলুন। যদি এই খাবারগুলি সমস্যার সৃষ্টি করে, তবে চিন্তা করবেন না - সুস্বাদু গ্লুটেন-মুক্ত বিকল্প উপলব্ধ রয়েছে। আপনাকে যা করতে হবে তা হল মুদি দোকান এবং স্বাস্থ্যকর খাবারের দোকানগুলি পরীক্ষা করা৷
ভাজা খাবার খেতে ভালোবাসেন? আমি আপনার জন্য খারাপ খবর আছে. নিয়মিত উচ্চ চর্বিযুক্ত খাবার খাওয়া শুধুমাত্র স্থূলতার মতো স্বাস্থ্য সমস্যা সৃষ্টি করে না তবে আইবিএস আক্রান্ত ব্যক্তিদের মধ্যে লক্ষণগুলিও বাড়িয়ে তুলতে পারে।
চিকিত্সকরা প্রায়শই ভাল অন্ত্রের কার্যকারিতার জন্য প্রতিদিন মোট চর্বি গ্রহণের পরিমাণ 40 - 50 গ্রামের বেশি সীমাবদ্ধ করার পরামর্শ দেন । পরিবর্তে চর্বিহীন প্রোটিন, ফলমূল, শাকসবজি এবং কম চর্বিযুক্ত দুগ্ধজাত খাবারের দিকে মনোযোগ দিন। এই ভারসাম্যপূর্ণ পদ্ধতির সামগ্রিক সুস্থতাও সাহায্য করে।
একটি IBS চিকিত্সা খাদ্য পরিকল্পনা বিরক্তিকর অন্ত্র সিন্ড্রোম নিয়ন্ত্রণে একটি অবিচ্ছেদ্য ভূমিকা পালন করে। আপনার খাদ্য অসহিষ্ণুতা আবিষ্কার করতে আপনার স্বাস্থ্যসেবা প্রদানকারীদের সাথে ঘনিষ্ঠভাবে কাজ করুন এবং অবিচ্ছিন্নভাবে অন্ত্র-বান্ধব খাবারে লেগে থাকুন।
নির্মূল ডায়েট পরীক্ষা করার সময় বা ধীরে ধীরে ফাইবার বাড়ানোর সময় সামঞ্জস্যের মাধ্যমে ধৈর্য ধরুন। দীর্ঘমেয়াদী হজম সুস্থতা অর্জন একটি যাত্রা, কিন্তু আপনি সেখানে পাবেন।
আপনার যদি আইবিএস থাকে তবে দুধ, পনির, আইসক্রিম এবং অন্যান্য দুগ্ধজাত খাবার এড়িয়ে চলুন কারণ ল্যাকটোজ গ্যাসের সমস্যা সৃষ্টি করে। এছাড়াও উচ্চ ফ্রুক্টোজ খাবার যেমন নির্দিষ্ট ফল, কার্বনেটেড পানীয় যা গ্যাসের প্রবর্তন করে, ক্যাফিন যা অন্ত্রকে উদ্দীপিত করে, এবং অশোষিত মিষ্টির সাথে চিনি-মুক্ত আঠা।
হ্যাঁ, আইবিএস ফ্লেয়ার-আপ বা ডায়রিয়া পর্বের সময় সাধারণ ভাত খাওয়া খুবই নিরাপদ। সহজে হজম হওয়া শস্যের লক্ষণগুলি খারাপ হওয়ার সম্ভাবনা নেই। মিষ্টি ছাড়া দুগ্ধজাত দুধও বেছে নিন, কারণ হজম করা কঠিন ল্যাকটোজ আপনার অন্ত্রকে আরও জ্বালাতন করতে পারে।
আইবিএস পরিচালনার জন্য আদর্শ খাদ্য পরামর্শ অন্তর্ভুক্ত:
https://www.health.harvard.edu/diseases-and-conditions/a-new-diet-to-manage-irritable-bowel-syndrome
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5548066
https://www.sciencedirect.com/science/article/abs/pii/S1542356515017152
Maintaining a healthy weight is not just about appearance; it’s about overall well-being. Diet plans play a pivotal role in achieving and sustaining weight goals, whether it’s shedding those extra pounds or gaining healthy mass. In this comprehensive guide, we delve into the intricacies of diet plans, exploring their significance, and benefits, and providing tailored strategies for weight loss and gain. Let’s embark on a journey toward a healthier you. if you need more information visit my website "https://leniloud.com/news/the-best-diet-plan-for-weight-loss-and-muscle-gain-in-2024/ "
A diet plan serves as a roadmap outlining your daily food intake, considering factors like calorie intake, macronutrient distribution, and meal timing.
https://leniloud.com/news/the-best-diet-plan-for-weight-loss-and-muscle-gain-in-2024/
মন্তব্য দেখানোর আগে অনুমোদিত হবে.
Portal Berita
অক্টোবর 19, 2024
Thank you for the information you have provided through your website,Portal Berita Telkom University you are very helpful.